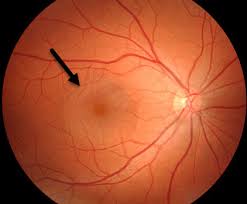
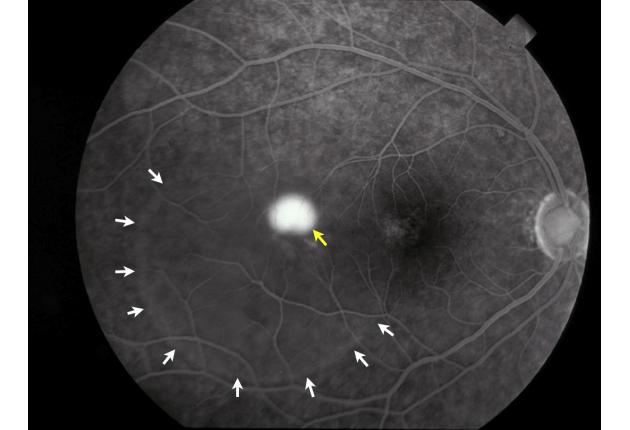
CENTRAL SEROUS CHORIORETINOPATHY (CSC)
Central serous chorioretinopathy is when fluid builds up under the retina. This can distort vision. The fluid leakage comes from a layer of tissue under the retina, called the choroid. The layer of cells between the retina and choroid is called the retinal pigment epithelium (RPE). When RPE does not work as it should, fluid builds up under the retina or the RPE resulting in a small detachment an
Who is in danger?
This is a common condition in adults 20-55 years old, men are 6 times more likely to get in than women. It is especially linked to psychological factors such as stress, type A personality, prolonged insomnia; or having a medical condition that requires corticosteroid use, increased blood pressure, sleep apnea. Several studies have linked Helicobacter pylori (the bacteria that cause gastric ulcer) and central serous chorioretinopathy - 78% people who have H. pylori also have the condition, compared to 43,5% of those who don’t.
How does the condition progress?
Prognosis of central serous chorioretinopathy is relatively good. 90% of patients can achieve the same vision as before the illness. However, chronic CSC has a poorer prognosis of vision due to diffuse pigment epithelial damage.
The disease has a good prognosis, but the recurrence rate is up to 40-50% and 5% of cases have complications of the pachychoroid neovasculopathy.
Can the condition be cured?
You need not be too worried because this disease is relatively benign, can be cured and does not leave any sequelae. You need to rest, avoid risk factors such as stimulants, alcohol, beer, tobacco, coffee, avoid nerve stress, and insomnia. You can embrace other static sports activities such as fishing, yoga.
Your doctor will prescribe medication to treat you, but you also need to keep track and revisit regularly to detect early if the disease recurs or if there are complications of the pachychoroid neovasculopathy.
If the condition is frequent and persistent, and your vision is deteriorating which affects your life, your doctor may perform a fluid probe laser. If there are complications of pachychoroid neovasculopathy, injections of anti-VEGF drugs are needed.

